
JUNE 2023
At Colorado Access, caring for you and your success is our top priority as you serve our members. This monthly Provider Update highlights important information and resources to help you as a contracted provider with us.
Public Health Emergency (PHE) Update
The PHE ends May 11, 2023. The renewal process for the more than 1.75 million people covered by either Health First Colorado (Colorado’s Medicaid program) or Child Health Plan Plus (CHP+) starts in May. The Colorado Department of Health Care Policy and Financing (HCPF) estimates that 30% of enrolled people will not need to take any action to remain covered, while the other 70% will need to submit eligibility verification.
HCPF also estimates that more than 325,000 people will no longer qualify for Health First Colorado and CHP+ coverage. People who no longer qualify can apply for insurance through the state’s official marketplace, Connect for Health Colorado, online or by calling their customer service line at 855-752-6749.
As more updates become available, we will continue to share what this means for you and for our members.
The PHE ended on May 11, 2023. Health First Colorado (Colorado’s Medicaid program) and Child Health Plan Plus (CHP+) members have returned to normal eligibility renewal processes. Noticing began in March 2023. The redetermination process will take place over 12 months, so not all members will have to renew at the same time. Members will be due for renewal in the calendar month they enrolled.
To ensure that you get properly reimbursed, you must check the Health First Colorado eligibility status of each of your patients:
At the time their appointment is scheduled
When they arrive for their appointment
If you have any questions, ask your practice facilitator. As more updates become available, we will continue to share what this means for you and for our members.
Click here to learn more.
Survey: Serious Mental Illness Practice Transformation Project
Mental Health Colorado is developing training and education materials to help providers better serve people with serious mental illnesses, including three brief surveys targeted towards different audiences to fully understand the needs of providers, people with lived experience of illness, and their loved ones. The surveys are open until Friday, June 23rd at 5:00 p.m.
The information they gather will be analyzed, evaluated, and shared over the next month. Your feedback is important. Please share the surveys with your network. If you have any questions or want to get more involved, email Bonnie Brandl at [email protected].
Telehealth Coverage Discontinued for Well Child Visits
Telehealth coverage for well child visits was added during the PHE, but this coverage was discontinued on May 12, 2023. You will still be reimbursed for in-person well child visits.
Click here to learn more.
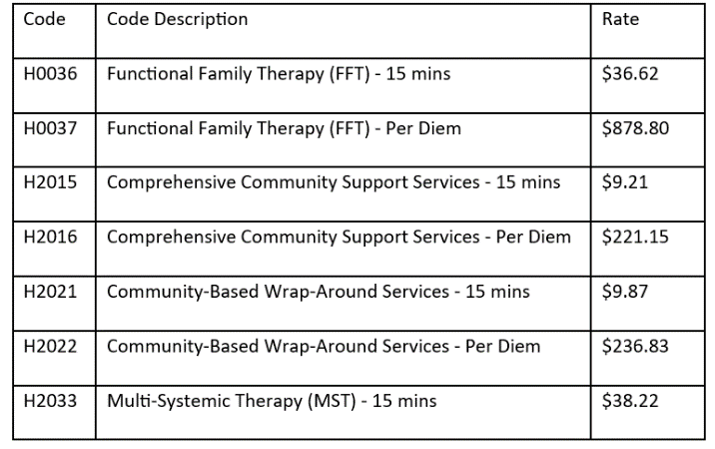
Health First Colorado Directed Payment Fee Schedule
Starting July 1, 2023, Health First Colorado will implement directed payments for certain child and adolescent behavioral health services. We will be sending you a notice of non-material change to your behavioral health fee schedule this month to comply with the directed payments. In addition to implementing directed Medicaid payments, we have applied the directed payments to the CHP+ fee schedule, and increased reimbursement for all CHP+ behavioral health services.
As a RAE, we have sole responsibility and discretion to contact with service providers and set provider rates, but Health First Colorado recognizes that there are unique situations where targeted action is necessary to support network access and growth for specific services. Directed payments will be established as a minimum reimbursement rate in these circumstances for specific services that RAEs must pay. We will be adequately funded to reimburse you at these rates when a directed payment is created. These will be time-limited investments that will be reviewed regularly.
Here is the fee schedule for directed payments. We are required to update provider contracts and claims systems to reflect a rate no less than these rates.
2023 Health Equity Plan Public Meetings
The Department of Health Care Policy and Financing (HCPF) has multiple health equity plan public meetings coming up. These meetings are for providers, members, and community stakeholders to learn more about the plan and give input and feedback.
For Opioid Treatment Providers: Take-Home Buprenorphine
As of May 1, 2023, a new policy began where opioid treatment providers (OTPs) may dispense up to a seven-day supply of take-home oral buprenorphine and buprenorphine combination physician-administered drugs (PADs) to Health First Colorado members. These PADs are to be billed through standard buy-and-bill processes when an OTP:
Get the appropriate Drug Enforcement Agency (DEA) registration
Has authority based on the rules and regulations set by the State of Colorado
Follows all guidelines set by the Substance Abuse and Mental Health Services Administration (SAMHSA)
Change to Adult Dental Benefit Limit for Health First Colorado
Starting July 1, 2023, Health First Colorado will remove the adult and Intellectual and Developmental Disabilities (IDD) dental benefit maximum. Members were previously limited to $1,500 a year, but there is no limit now. All services will be covered at 100%. This does not affect frequency; those limits remain the same.
CHP+ Breast Pump/Lactation Benefit
As of July 1, 2022, CHP+ offered by Colorado Access has a benefit that covers breast pumps for prenatal and postpartum CHP+ members. If you are a Durable Medical Equipment, Prosthetics, Orthotics, and Supplies (DMEPOS) provider, you may now bill us as the primary payer for manual and/or single user electric breastfeeding pumps.
Before July 1, 2022, Women, Infants, and Children (WIC) was the primary payer for breast pumps for Health First Colorado and CHP+ members, but now members may get a breast pump from either Colorado Access or WIC.
Single-User Breast Pumps
The rate for procedure code E0603 for electric breast pumps is $133.30.
The rate for procedure code E0602 for manual breast pumps is $20.47.
Prior authorization requests (PARs) are not required.
Members may get a breast pump as early as the 28th week of their pregnancy. If the member delivers before 28 weeks, they qualify for a breast pump immediately after the birth.
Postpartum members may get a pump at any time.
Breast pumps may be prescribed by a physician, physician assistant, nurse practitioner, or certified nurse midwife. A prescription is required.
Claims will not be denied based on the diagnosis code used. Diagnosis code Z39.1 is appropriate.
A single user collection kit specifically made for the corresponding pump must also be given to each user and should not be billed separately.
Multi-User Breast Pumps
When billing for multi-user breast pumps, use procedure code E0604 with modifier RR.
As of January 1, 2023, the reimbursement rate is $219.67.
This is a continuous rental item that will not be converted to purchase.
Prescriptions should include information on why a single-user pump is not enough for the member.
You are required to give the member any necessary material and training on appropriate cleaning, storage, and use. You must also give the member a single user collection kit specifically made for the corresponding pump. This should not be billed separately.
Additional accessories and supplies needed during the usage period, including replacement parts, are inclusive of the monthly rate and should not be billed separately.
All rented pumps must be approved by the Food and Drug Administration (FDA) as a multi-user breast pump.
Members may get a breast pump as early as the 28th week of their pregnancy. If the member delivers before 28 weeks, they qualify for a breast pump immediately after the birth.
If the member’s doctor says they need a stronger or hospital-grade pump, the member can rent one by following the same process to get a prescription.
Hospital-grade pumps are rented through an in-network hospital, instead of a DME provider. They may be rented for up to two years. The member must return the pump when they no longer need it.
Family Planning Updates
Starting July 1, 2023, members in the emergency medical services (EMS) and reproductive health care program category are eligible to get family planning-related services for a $0 copay, which will expand the services this population is eligible for.
Family planning-related services are those that are provided with a family planning visit. Click here to learn more about the definition of these services. The expansion in this coverage is in addition to the existing coverage of emergency services, which has separate billing guidance.
Free Screening, Brief Intervention and Referral to Treatment (SBIRT) Training
If you are a Health First Colorado provider, you can get free SBIRT training through a partnership with Peer Assistance Services, Inc. (PAS). This program promotes prevention and early intervention efforts through training (in-person, online, and virtual), technical assistance, and hands-on SBIRT implementation. Learn more here.
Click here to register for an upcoming training.
If you have any questions, email Janelle Gonzalez at [email protected].
Senate Bill (SB) 21-137 Implementation
SB 21-137, Behavioral Health Recovery Act of 2021, Section 9, will be implemented July 1, 2023. The full bill was signed into law in Colorado in 2021. It requires that the Department of Health Care Policy and Financing (HCPF) get a second medical necessity review for residential or inpatient substance use disorder (SUD) requests. HCPF’s utilization management vendor, Kepro®, will perform the second SUD reviews.
There must be a second review if a provider enrolled in Health First Colorado requests it when a Regional Accountable Entity (RAE) denies or reduces SUD services, and the member’s appeal to reverse that decision is denied by a Colorado administrative law judge. SB 21-137 requires a provider to sponsor the request for the second medical necessity review. You can submit an SB 137 Section 9 request form for this, which will soon be available here.
There is also a process for members to initiate a second review. Members must give contact information for a Health First Colorado provider who will sponsor the request. To initiate a second review, the member should email their name and contact information to [email protected]. They will be contacted for more information about the original SUD denial and the name of their provider, and the identified provider will be contacted with instructions on how to formally request the second SUD review.
Click here to learn more.
411 Behavioral Health Audit
The annual state mandated 411 behavioral health audit has been completed. A total of 1233 claims across the state of Colorado were reviewed. Documentation was audited across three behavioral health service categories – inpatient, residential and outpatient psychotherapy. Providers involved in this audit should expect to receive results letters in July 2023. In the meantime, the COA Compliance Department is working hard on collaborating internally to incorporate more education and training opportunities to help support providers.
